Episode 144: Myeloma Series, Pt. 5 - Myeloma Risk Stratification and Response Criteria (2026)
This week, we introduce a new episode for our myeloma series, this time focusing on risk stratification and response criteria. The initial workup and surveillance labs are expansive, but all of the studies we do have a purpose.
Many present-day studies also use “minimal residual disease” (MRD) testing. What does this mean? How do we use this?
We go through all of this and more in this incredibly high yield episode.
A quick reminder on high risk MGUS:
Abnormal serum free light chain
Serum M-protein >1.5 g/dL
Non-IgG M-spike
For a more thorough discussion, be sure to check out episode 141
Breaking down the bone marrow biopsy
Aspirate
The liquid part of the marrow:
Able to get a smear and cell counts
Allow us to run flow and cytogenetic testing
Core
The solid, trabecular part of the marrow.
Provides information on marrow structure and cellularity
Able to run immunohistochemistry (IHC) which measures protein expression on fixed tissue to allow estimation of % of abnormal cells in bone marrow
How do we determine the % of plasma cells in the bone marrow?
It involves a combination of techniques including IHC on the core and flow cytometry on the aspirate both allowing for estimates of abnormal clonal populations with kappa or lambda restrictions.
What are the new updated criteria for high risk MM?
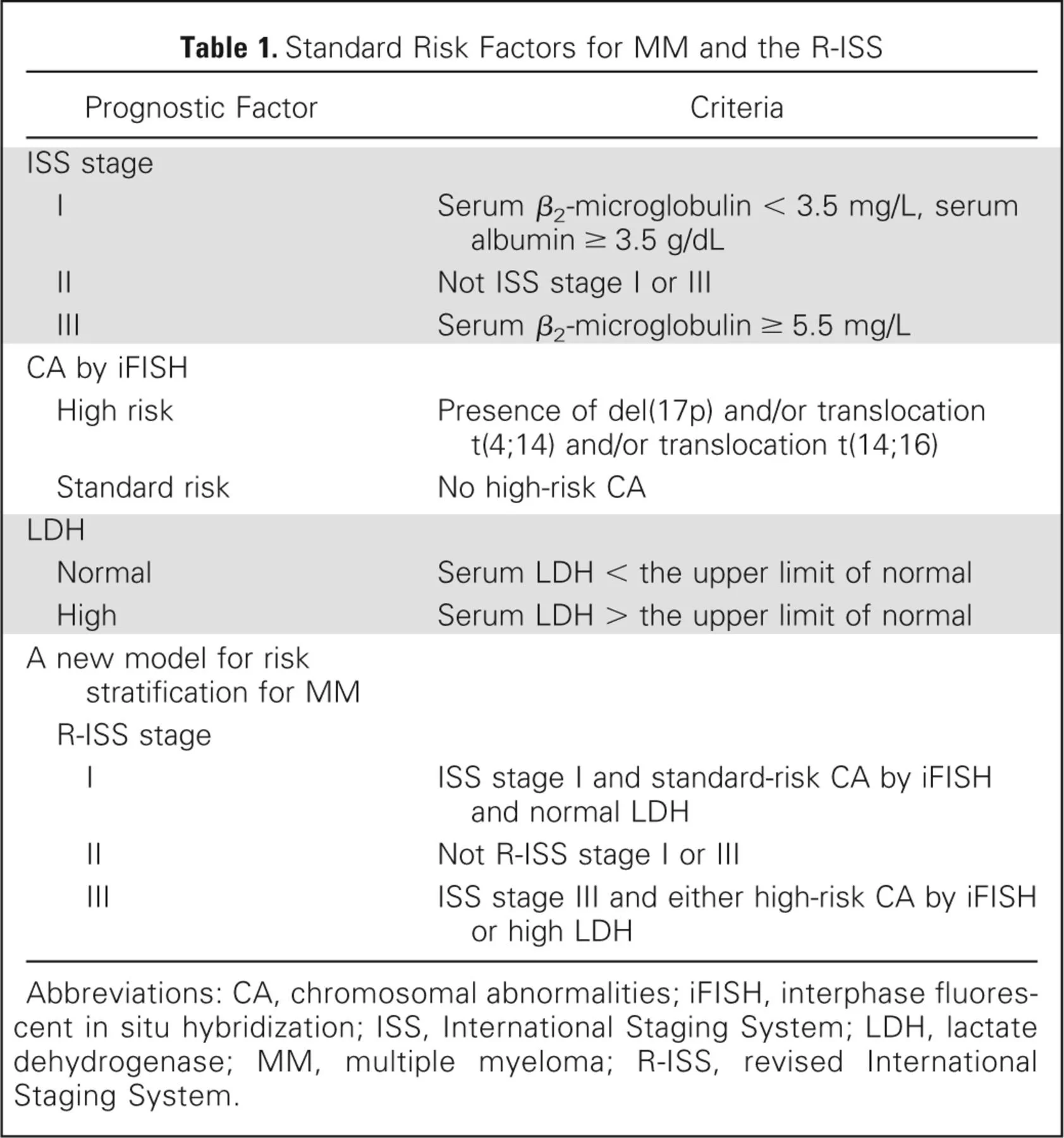
The 2015 updated definition from the International Myeloma Working Group refines how we identify patients with high risk MM at the highest risk for progression and death. Note that this system includes high risk cytogenetics into the risk stratification. These updates build on prior staging system, known as the Durie-Salmon staging system.
Image source: Table 1. Palumbo et al. J Clin Oncol 33, 2863-2869(2015), Volume 33, Number 26, DOI: 10.1200/JCO.2015.61.2267
High risk features:
Deletion 17p (>20% clonal fraction)
IGH translocation of one of the following loci: t(4;14), (14;16), t(14;20)
Biallelic del(1p32) or monoallelic del(1p32) with concurrent 1q gain
B2 Microglobulin >5.5 with normal renal function
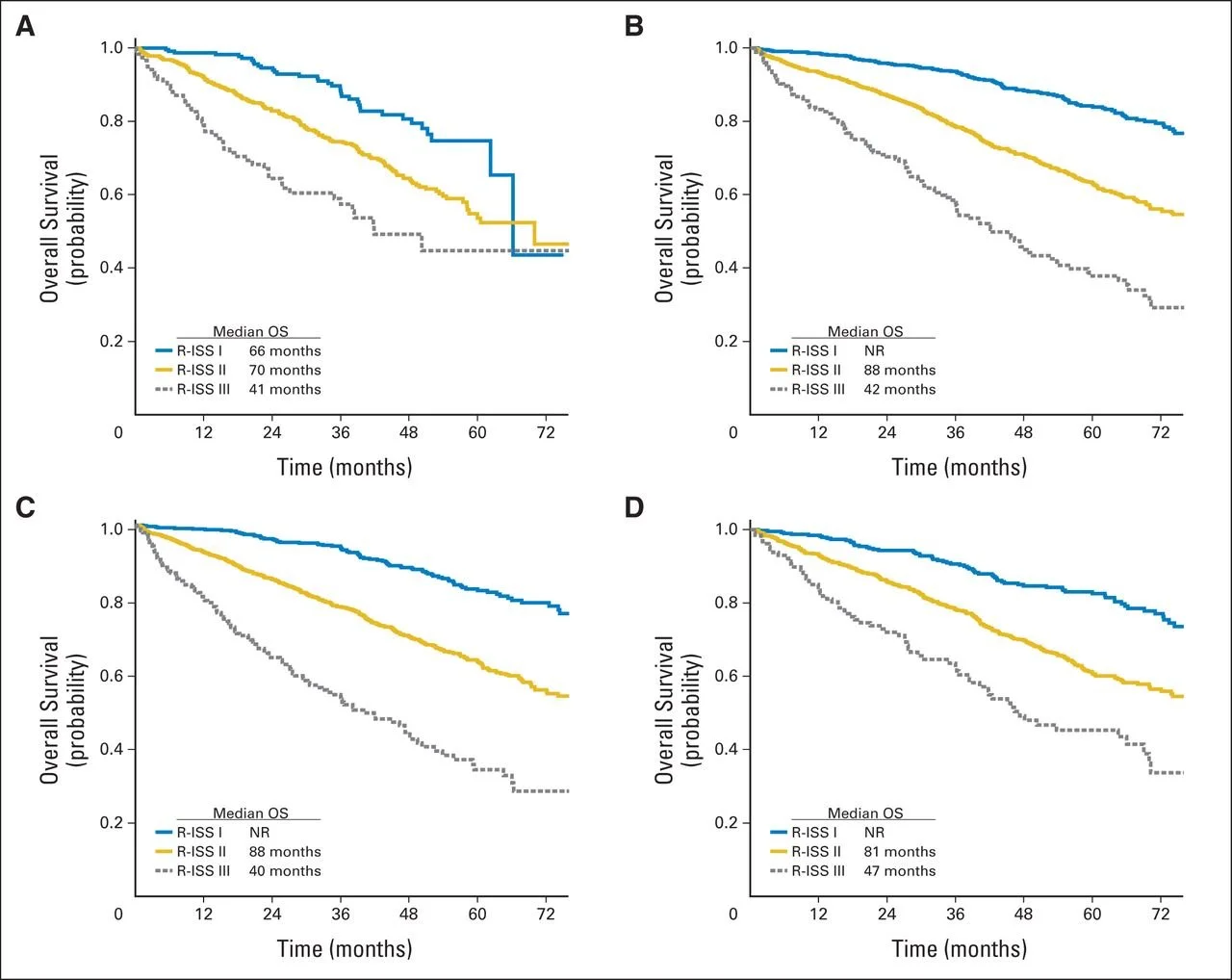
The figure below shows how the updated R-ISS categories clearly result in a separation of the overall survival curves (OS).
Image source: Figure 3. Palumbo et al. J Clin Oncol 33, 2863-2869(2015), Volume 33, Number 26, DOI: 10.1200/JCO.2015.61.2267
What do the response criteria mean for MM?
The IMWG has a consensus for the various response criteria linked here.
Partial response (PR)
Very good partial response (VGPR)
Complete Response (CR)
Stringent Complete Response (sCR)
MRD negative
VGPR
Defined by detectable M spike by IFE but unable to quantify OR >90% reduction in M spike from baseline and <100 mg of monoclonal protein in 24 hour UPEP
This is an example of when you would repeat a 24 hour UPEP to assess response only if there was a UPEP quantification at baseline
Note that FLC ratio does not have to be normal
PR
Just remember 50% and this also emphasizes why 24 UPEP baseline and imaging is important for disease monitoring
50% reduction in M spike and >90% reduction in urinary 24 hour M protein or to <200 mg/24 hours
If no M spike and light chain only disease, then 50% reduction in FLC ratio
If no M spike or FLC, then 50% reduction in BMPC percentage
Also always need 50% reduction in plasmacytoma if present at baseline
CR and sCR requires bone marrow biopsy
CR means no M spike and <5% clonal plasma cells
sCR means no M spike, normal FLC ratio, and no clonal population of plasma cells on marrow
A level of CR or deeper requires a repeat marrow evaluation which often is done after ~4 cycles of therapy in transplant eligible patients
Ideally time to collect stem cells is ~cycle 4
Progressive Disease: Progression can be asymptomatic lab value progression. The trajectory of these labs matter.
>25% increase from the lowest response value or nadir in one of the following:
Serum M-component and/or (absolute increase must be > 0.5 g/dL)
Urine M-component and/or (absolute increase must be > 200 mg/24 h)
In patients without measurable serum and urine M-protein levels the increase of involved and uninvolved FLC levels >100 mg/L.
Bone marrow plasma cell percentage >10%
Development of new bony lesions or plasmacytomas OR increase in existing lesions.
Development of hypercalcemia (corrected serum calcium > 11.5 mg/dL) attributable to MM
What role does MRD testing play in MM?
Minimal residual disease (MRD) testing is an emerging test which is highly sensitive in detecting residual myeloma beyond the typical response criteria above, looking more granular at the specific plasma cell clones that may not be currently causing clinical disease. This article highlights differences between the various MRD testing.
Next-Generation Flow Cytometry (NGF)
NGF uses flow cytometry to identify abnormal plasma cells based on their immunophenotype.
Sensitivity: 1 in 1,000,000 cells
Strengths: Highly sensitive, fast return
Limitations:
Requires live, viable cells that must be processed within 24-48 hours
Cannot determine clonal evolution because only looking at the cell surface proteins
Next Generation Sequencing (NGS)
NGS MRD testing uses molecular sequencing of the immunoglobulin gene rearrangements actually looking specifically at the patient's initial bone marrow to identify clonal populations. In NGS-based MRD assessment, the IgH/IgK/IgL loci are sequenced to capture Ig gene re-arrangements in residual MM cells. The NGS data could be further interpreted to identify subclones, clonal evolution, and cloning tides at the MRD stage.
Sensitivity: 1 in 1,000,000 cells (with some data suggesting it may be even sensitive to 1 in 10,000,000 cells)
Strengths:
Does not require immediate processing
Allows assessment of clonal evolution and subclonal development
Captures nearly all immunoglobulin gene rearrangements
Uses a standardized, universal platform
Limitations:
Expensive and resource intensive
Longer turnaround time (on average 5 days to 2 weeks)
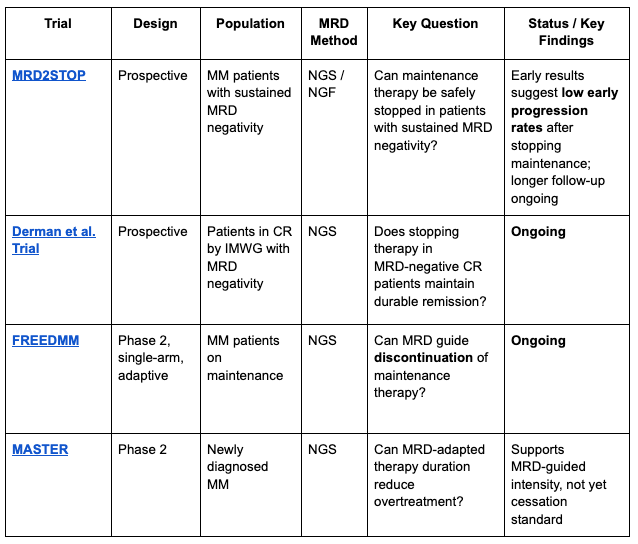
What does this mean for clinical practice?
Unclear what this currently means for clinical practice. There are various trials looking at this exact question.
While MRD appears to be a positive signal, we do not have enough data to discontinue therapy, though many trials are actively trying to determine this.
Early signals suggest that deep durable MRD negativity could allow for cessation of maintenance therapy.
References
Antonio Palumbo et al. Revised International Staging System for Multiple Myeloma: A Report From International Myeloma Working Group. J Clin Oncol 33, 2863-2869(2015). DOI:10.1200/JCO.2015.61.2267
International Myeloma Working Group. International Myeloma Working Group (IMWG) uniform response criteria for multiple myeloma. International Myeloma Foundation. Accessed 12/30/2025. https://www.myeloma.org/resource-library/international-myeloma-working-group-imwg-uniform-response-criteria-multiple
Ben A. Derman, Ajay Major, Sarah Major, Brittany D. Wolfe, Martha Gorski, Jennifer H. Cooperrider, Evangelia Andreatos, Ken Jiang, Karson Buckley, Amanda McIver, Andrew Stefka, Andrzej Jakubowiak; Prospective Trial Using Multimodal Measurable Residual Disease Negativity to Guide Discontinuation of Maintenance Therapy in Multiple Myeloma (MRD2STOP). Blood 2022; 140 (Supplement 1): 2108–2109. doi: https://doi.org/10.1182/blood-2022-158643
Karen Sweiss, Craig C Hofmeister, Maria Zappia, Maxim Frolov, Elizaveta Benevolenskaya, John G. Quigley, Shrihari Kadkol, Douglas W. Sborov, Damiano Rondelli, Pritesh Patel; Free from Maintenance Drug Therapy in Multiple Myeloma (The FREEDMM Trial): A Pilot Study of Minimal Residual Disease (MRD)-Driven Discontinuation of Maintenance. Blood 2022; 140 (Supplement 1): 7304–7305. doi: https://doi.org/10.1182/blood-2022-170936
Neha Korde, Benjamin Diamond, Miranda Burge, Hani Hassoun, Heather Landau, Malin Hultcrantz, Sham Mailankody, Kylee H Maclachlan, Urvi A Shah, Andriy Derkach, Saad Usmani, Ola Landgren, Alexander Lesokhin; Maintenance Therapy Cessation for Sustained MRD Negative Multiple Myeloma Patients. Blood 2022; 140 (Supplement 1): 2397–2398. doi: https://doi.org/10.1182/blood-2022-169937
The crew behind the magic:
Show outline: Vivek Patel, Sean Taasan
Production and hosts: Ronak Mistry, Vivek Patel, Dan Hausrath, Sean Taasan
Editing: Resonate Recordings
Shownotes: Megan Connor
Graphics, social media management: Ronak Mistry