Episode 145: Myeloma Series, Pt. 6 - First line treatment of Multiple Myeloma (2026)
This week, we begin our discussion about treatment of multiple myeloma, focusing on the first-line setting. Once again, a lot has changed in this space over the last few years, most notably the standards of care (now quadruplet regimens instead of triplet regimens!). We break down the data and how to help you practically approach your treatment planning for your patient with newly diagnosed multiple myeloma.
This episode is brought to you by Primum! To learn more, sign up for your free account, and to ask questions to Primum experts, click here!
What are the phases of treatment for multiple myeloma?
Induction
Goal: Attempting to debulk disease
Usually with 4-6 cycles of therapy with aim to achieve at least a partial response (PR), which is at least a 50% reduction in the M-spike; ideally, aiming for very good partial response (VGPR)
For refresher on response criteria, check out episode 144
We collect stem cells during induction therapy before the bone marrow is too damaged from repeated rounds of chemotherapy.
Bone marrow plasma percentage ideally < 10% when thinking about transplant
Consolidation
Goal: Deepen our response with more therapy
In transplant eligible patient: You are trying to do this with high doses of chemotherapy (alkylator), specifically melphalan 200mg/m2 (“Mel 200”)
What is the basic principle here? Attacking the patient’s myeloma with a very myeloablative regimen, which causes so much toxicity that it cannot recover on it’s own. Therefore the autologous stem cell transplant is the rescue
In transplant ineligible patient: We can consolidate with more cycles of our induction therapy or slightly more intense regimens compared to maintenance
Maintenance
Goal: Use lower dose of therapy to maintain response, minimize toxicity and maximize the patient’s quality of life.
Most commonly see patients on oral revlimid (lenalidomide), daratumumab + revlimid or Bortezomib + revlimid
Hopeful to soon have fixed duration maintenance but often maintenance therapy is indefinite
Relapsed Refractory
More on this in a future episode. Spoiler alert: there’s many options
How do we know if a patient is quadruplet induction eligible and transplant eligible?
In order literature (and even in our original myeloma series!) you may hear that the first branch point was “transplant eligible” or “transplant ineligible”. Refer back to previous Episode 044: Myeloma series, pt. 5 - Myeloma Treatment; however, in 2026, the first step is determining if patients are “quadruplet induction eligible” or “quadruplet induction ineligible”
Decision impacted by patients’ functional status and fitness
Transplant eligibility
Patients eligible generally are <75yrs of age (no technical age cutoff), based on physiologic reserve and the absence of major comorbidities
For Patients 65-70 yrs of age you will see often see reduced doses of melphalan 140mg/m2 (“Mel 140”)
“Mel 140” also used for patients with renal dysfunction
Take home point - patients that are fit for major surgery are likely fit for transplant
Quadruplet eligibility
No good established guidelines
Fitter patients that are independent and walk regularly, even candidates in their 80s (ongoing randomized trials to determine if improved OS in this population)
What does triplet or quadruplet induction therapy mean?
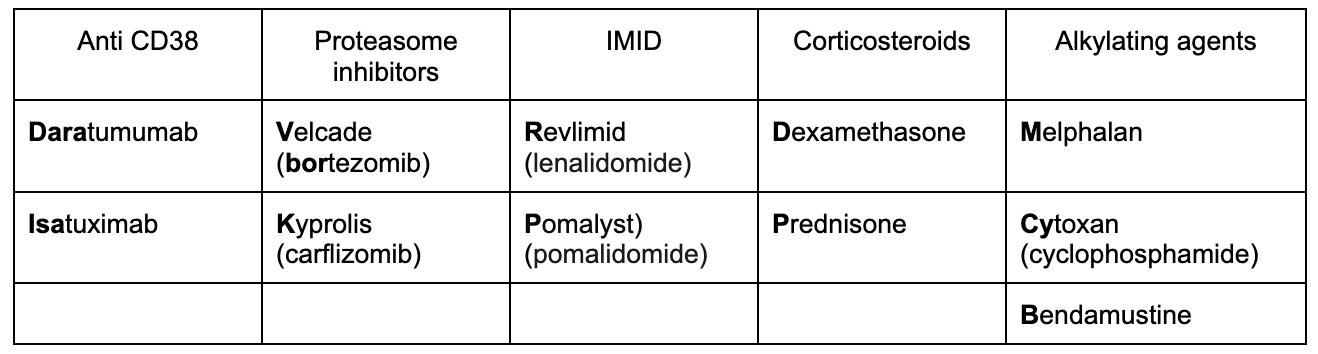
We combine multiple classes of medications (3 or 4). Refer to Episode 143: Myeloma Series, Pt 4 - Myeloma Pharmacology for a review
All patients should get a backbone of an anti-CD38 monoclonal antibody (daratumumab or isatuximab) and dexamethasone in their treatment regimen
After that we either add one drug or two additional drugs to get to the triplet or quadruplet
Triplet: anti-CD38 + dexamethasone + EITHER immunomodulatory drug (IMID) OR proteosome inhibitor
IMIDs: “Omide” drugs; examples: lenalidomide (Revlimid), pomalidomide (Pomalyst)
Proteosome inhibitors: “Zomib” drugs; examples: bortezomib (Velcade) or carflizomib (Kyprolis)
Quadruplet: anti-CD38 + dexamethasone + immunomodulatory drug + proteosome inhibitor
For those with severe renal dysfunction may see alkylator (Cyclophosphamide) instead of an IMID in the inpatient setting
Table created by Matthew Barke, MD
What is high risk myeloma?
For an in-depth discussion on risk stratification, refer back to episode 144: Myeloma Series, Pt. 5 - Myeloma Risk Stratification and Response Criteria
R-ISS: Used LDH, albumin and beta 2 microglobulin for risk stratification
Elevated LDH and beta 2 microglobulin are poor prognostic factors (particularly if >5.5)
IMWG 2025 Update - high risk defined primarily by cytogenetics
Deletion 17p (>20% clonal fraction) or TP53 mutation (17p is where p53 locus exists)
IGH translocation of one of the following loci: t(4;14), (14;16), t(14;20) along with del 1p or gain 1q
Biallelic del(1p32) or monoallelic del(1p32) with concurrent 1q gain
B2 Microglobulin >5.5 with normal renal function
How did we get to our current treatment standards of care?
In our prior episode, we discussed the history of how we got to our current treatment standards of care. Interested to learn more? Refer back to episode 045: Myeloma Series, Pt. 6 - Myeloma Treatment in Transplant Ineligible Patients for comprehensive historical perspective
Briefly, the fascinating highlights are as follows:
-
MP, that is, Low dose oral Melphalan (an alkylating agent) and Prednisone was the standard of therapy for Multiple Myeloma.
Progression free survival with MP was 15 months, overall survival very poor.
-
High dose IV Melphalan + dexamethasone followed by stem cell transplant (as high dose melphalan resulted in bone marrow failure).
For relapse refractory disease after MP, high dose dexamethasone alone was given.
The efficacy of dexamethasone in myeloma treatment has been known for a long time. (This is why high dose dex is still included in all myeloma regimens today!)
-
MP was still the standard of care.
Thalidomide was used for relapse/refractory disease for its anti-angiogenic properties.
It was removed from the market due to its teratogenic properties (severe limb hypoplasia in fetus) when given to pregnant women. Later, it was approved for myeloma treatment.
Newer generations are now used including Lenalidomide (Revlimid) and Pomalidomide, which have lesser toxicity but are more expensive.
Thalidomide is still used around the world, especially in Europe, but newer agents are more popular in the US.
Around the same time, Bortezomib was introduced.
It is a dipeptide which has boronic acid component (hence the name “Bor” tezomib). It was the first ever proteasome inhibitor used for Myeloma treatment.
Original studies looked at Velcade vs dex in relapsed/refractory settings, getting its approval.
Cytotoxic chemotherapy was also used as induction therapy prior to transplant. Commonly a combination of vincristine + doxorubicin (aka Adriamycin) + dexamethasone (VAD). Studies in the relapsed/refractory setting suggested that dexamethasone was doing the heavy lifting in these regimens.
Multiple trials used combinations of IMID + proteosome inhibitors -> IMID in frontline setting found to better than chemotherapy
As a result, later studies found doublets velcade + dexamethasone and thalidomide + dex to be more efficacious than the cytotoxic regimens.
IFM 2005-01 Phase III Trial compared Velcade + dexamethasone to vincristine + doxorubicin + dexamethasone and found velcade + dexamethasone had better VGPR rates and less toxicity
-
Numerous trials looked at a variety of doublet and triplet combinations.
SWOG S0777 trial: Randomized patients to VRd (Velcade/Revlimid/Dexamethasone) induction vs Rd (Revlimid/Dexamethasone); Triplet improved OS for both transplant eligible and ineligible patients
Median PFS was significantly improved in the VRd group 43 months vs 30 months in the Rd group
Median OS for VRd 75 months vs 64 months in the Rd group
Take home point: VRd becomes standard of care
Development of 2nd generation of proteasome inhibitor carflizomib (Kyprolis) so VRd becomes KRd
ENDURANCE phase III trial (E1A11)
Compared KRd vs VRd
Included both transplant eligible and ineligible patients. Excluded high risk patients from the trial
No difference in PFS or OS
More cardiopulmonary toxicity, renal toxicity, and treatment related deaths in KRd arm
VRd arm with more neuropathy ~8% of patients
Randomized 1:1:1 to either KCyD, KRd without transplant and KRd consolidation, or KRd with transplant
Second randomization to KR vs. R maintenance
KRd 70% vs. KCyD 50%
Carfilzomib-based induction, intensification, consolidation regimens are effective strategies in patients with standard risk and high-risk myeloma
-
Compared quadruplet induction Dara-VRd vs triplet VRd for transplant eligible patients
Primary endpoint was stringent CR after autologous transplant + 2 more cycles of consolidation therapy with dara-VRD or VRD
4-year PFS was 87% for D-VRd vs 70% for VRd
Addition of daratumumab to VRd improved the depth of response and progression-free survival in transplantation-eligible patients with newly diagnosed multiple myeloma
PERSEUS phase III trial examine quadruplet induction Dara-VRd vs triplet VRd;
Over 700 transplant eligible patients were randomized to Dara-VRd vs. VRd
PFS at 48 months was 84.3% in the Dara-VRd group and 67.7% in the VRd group
MRD-negative status (58% Dara-VRd vs. 33% VRd)
Take home point: Dara-VRd is now standard
What is Trial Level Surrogacy?
EVIDENCE meta analysis: Achieving MRD negativity improved PFS as a surrogate endpoint
If we look at each trial individually: what is the Δ MRD negativity compared to Δ PFS and see if they correlate
Each Δ MRD negativity correlated to Δ PFS in each trial
What is the role of Carfilzomib in quadruplet induction therapy?
MASTER phase II trial: One pivotal MRD adapted trial incorporating carfilzomib was the Multicenter Single Arm Phase II MASTER Trial
All patients got Dara-KRD induction
Primary endpoint was MRD negativity
Goal was a risk adapted approach with surveillance for MRD negative patients instead of revlimid maintenance
70% of patients achieved MRD negativity on two consecutive measurements with only 4% resurgence of disease without maintenance therapy in lower risk patients
High risk patients had worse outcomes with 27% resurgence of disease without maintenance therapy
Proof of concept for future myeloma studies: two consecutive MRD negative measurements then drop maintenance therapy
Over 300 patients were randomized to either Isa-KRd or KRd
Primary endpoint was MRD negativity after consolidation
MRD negative rate was a 77% Isa-KRd vs. 67% KRd after transplant consolidation
MRD negative rate after induction was 46% Isa-KRd vs. 26% KRd
These are numerically higher than PERSEUS but it is critical that we do not make cross trial comparisons so without a phase III randomized trial we can’t draw too many conclusions
There’s no evidence that isatuximab which is notably IV is better than more convenient subcutaneous daratumumab
What do we do for quadruplet ineligible patients?
Remember there is a gray zone for quadruplet induction eligible but this is definitely less strict than transplant eligible
The biggest concern is the risk of infection and associated complications that come with hospitalization from infection with quadruplet induction vs. triplet induction
For a patient that may be frail and with multiple comorbidities (not quadruplet eligible) common triplet regimen is Daratumumab, revlimid and dexamethasone (dara-Rd)
This was first evaluated in the pivotal phase III MAIA trial published in NEJM 2019
Included over 700 patients randomized to Dara-Rd vs. Rd
It is unclear why RVd was not the control arm
5 year PFS was over 60% in the Dara-Rd arm vs. 30% in the Rd arm
There were two similar quad vs. triplet studies: CEPHEUS and IMROZ
CEPHEUS phase III trial: looked at Dara-VRd followed by Dara-R maintenance vs. VRd followed by R maintenance in transplant ineligible patients
Primary endpoint was MRD negativity which was obviously improved with quadruplet (61% in quadruplet arm vs 39% in triplet arm)
Roughly 5 year PFS was 68% in the quadruplet arm vs. 50% in the triplet arm
IMROZ phase III trial: looked at Isa-VRd vs. VRd in transplant ineligible patients
5 year PFS of 63% in Isa-VRd arm vs. 45% in the VRd triplet
More side effects with addition of anti CD38
More grade 3 or higher infections at 45% vs. 38%
Double the rate of infections leading to death at 6% vs. 3%
Randomized patients to Isa-VRd vs. Isa-Rd
Excluded patients above the age of 79 which limits the generalizability to some of our older myeloma population
Improved MRD negativity and response rates
18-month MRD negativity: Isa-VRd 53% vs 26% for Isa-Rd
18 month complete response: Isa-VRd 58% vs 33% for Isa-Rd
No difference in PFS or OS though data are immature
They did not report grade or higher infections but simply grade 2 or higher which is a huge limitation
Take home point: Quadruplet will maximize PFS but there is a higher risk of infection with quadruplet therapy so choose patients wisely
This episode is brought to you by Primum! To learn more and sign up for free, click here!
References
Hervé Avet-Loiseau et al. International Myeloma Society/International Myeloma Working Group Consensus Recommendations on the Definition of High-Risk Multiple Myeloma. J Clin Oncol 43, 2739-2751(2025). DOI:10.1200/JCO-24-01893
Jean-Luc Harousseau et al. Bortezomib Plus Dexamethasone Is Superior to Vincristine Plus Doxorubicin Plus Dexamethasone As Induction Treatment Prior to Autologous Stem-Cell Transplantation in Newly Diagnosed Multiple Myeloma: Results of the IFM 2005-01 Phase III Trial. J Clin Oncol 28, 4621-4629(2010). DOI:10.1200/JCO.2009.27.9158
Durie BGM, Hoering A, Abidi MH, et al. Bortezomib with lenalidomide and dexamethasone versus lenalidomide and dexamethasone alone in patients with newly diagnosed myeloma without intent for immediate autologous stem-cell transplant (SWOG S0777): a randomised, open-label, phase 3 trial. Lancet. 2017;389(10068):519-527.
Kumar SK, Jacobus SJ, Cohen AD, et al. Carfilzomib or bortezomib in combination with lenalidomide and dexamethasone for patients with newly diagnosed multiple myeloma without intention for immediate autologous stem-cell transplantation (ENDURANCE): a multicentre, open-label, phase 3, randomised, controlled trial. Lancet Oncol. 2020;21(10):1317-1330. doi:10.1016/S1470-2045(20)30452-6
Gay F, Musto P, Rota-Scalabrini D, et al. Carfilzomib with cyclophosphamide and dexamethasone or lenalidomide and dexamethasone plus autologous transplantation or carfilzomib plus lenalidomide and dexamethasone, followed by maintenance with carfilzomib plus lenalidomide or lenalidomide alone for patients with newly diagnosed multiple myeloma (FORTE): a randomised, open-label, phase 2 trial. Lancet Oncol. 2021;22(12):1705-1720. doi:10.1016/S1470-2045(21)00535-0
Voorhees PM, Sborov DW, Laubach J, et al. Addition of daratumumab to lenalidomide, bortezomib, and dexamethasone for transplantation-eligible patients with newly diagnosed multiple myeloma (GRIFFIN): final analysis of an open-label, randomised, phase 2 trial. Lancet Haematol. 2023;10(10):e825-e837. doi:10.1016/S2352-3026(23)00217-X
Sonneveld P, Dimopoulos MA, Boccadoro M, et al. Daratumumab, Bortezomib, Lenalidomide, and Dexamethasone for Multiple Myeloma. N Engl J Med. 2024;390(4):301-313. doi:10.1056/NEJMoa2312054
Landgren O, Prior TJ, Masterson T, et al. EVIDENCE meta-analysis: evaluating minimal residual disease as an intermediate clinical end point for multiple myeloma. Blood. 2024;144(4):359-367. doi:10.1182/blood.2024024371
Costa LJ, Chhabra S, Medvedova E, et al. Minimal residual disease response-adapted therapy in newly diagnosed multiple myeloma (MASTER): final report of the multicentre, single-arm, phase 2 trial. Lancet Haematol. 2023;10(11):e890-e901. doi:10.1016/S2352-3026(23)00236-3
Gay F, Roeloffzen W, Dimopoulos MA, et al. Results of the Phase III Randomized Iskia Trial: Isatuximab-Carfilzomib-Lenalidomide-Dexamethasone Vs Carfilzomib-Lenalidomide-Dexamethasone As Pre-Transplant Induction and Post-Transplant Consolidation in Newly Diagnosed Multiple Myeloma Patients. Blood 2023; 142 (Supplement 1): 4. doi: https://doi.org/10.1182/blood-2023-177546
Facon T, Kumar S, Plesner T, et al. Daratumumab plus Lenalidomide and Dexamethasone for Untreated Myeloma. N Engl J Med. 2019;380(22):2104-2115. doi:10.1056/NEJMoa1817249
Usmani SZ, Facon T, Hungria V, et al. Daratumumab plus bortezomib, lenalidomide and dexamethasone for transplant-ineligible or transplant-deferred newly diagnosed multiple myeloma: the randomized phase 3 CEPHEUS trial. Nat Med. 2025;31(4):1195-1202. doi:10.1038/s41591-024-03485-7
Facon T, Dimopoulos MA, Leleu XP, et al. Isatuximab, Bortezomib, Lenalidomide, and Dexamethasone for Multiple Myeloma. N Engl J Med. 2024;391(17):1597-1609. doi:10.1056/NEJMoa2400712
Leleu X, Hulin C, Lambert J, et al. Isatuximab, lenalidomide, dexamethasone and bortezomib in transplant-ineligible multiple myeloma: the randomized phase 3 BENEFIT trial. Nat Med. 2024;30(8):2235-2241. doi:10.1038/s41591-024-03050-2
The crew behind the magic:
Show outline: Vivek Patel, Sean Taasan
Production and hosts: Ronak Mistry, Vivek Patel, Dan Hausrath, Sean Taasan
Editing: Resonate Recordings
Shownotes: Matt Barke
Graphics, social media management: Ronak Mistry