Episode 140: Myeloma Series, Pt.1 - Intro to Testing and MGUS (2025)
It’s been 3 years since our last myeloma series updates and the reality is, a lot has changed! Instead of releasing an updates episode, we are redoing our prior myeloma series to make sure that you, our listeners, can follow along the way you always have.
In the first episode in our highly-anticipated multiple myeloma series, we begin our discussion about introduction to testing/workup for plasma cell dyscrasias and having our initial discussion about monoclonal gammopathy of undetermined significance (MGUS).
What is the function of a plasma cell?
Plays role in humoral immunity in producing antibodies
Normally, your body will have an elevation of many different immunoglobulins/antibodies
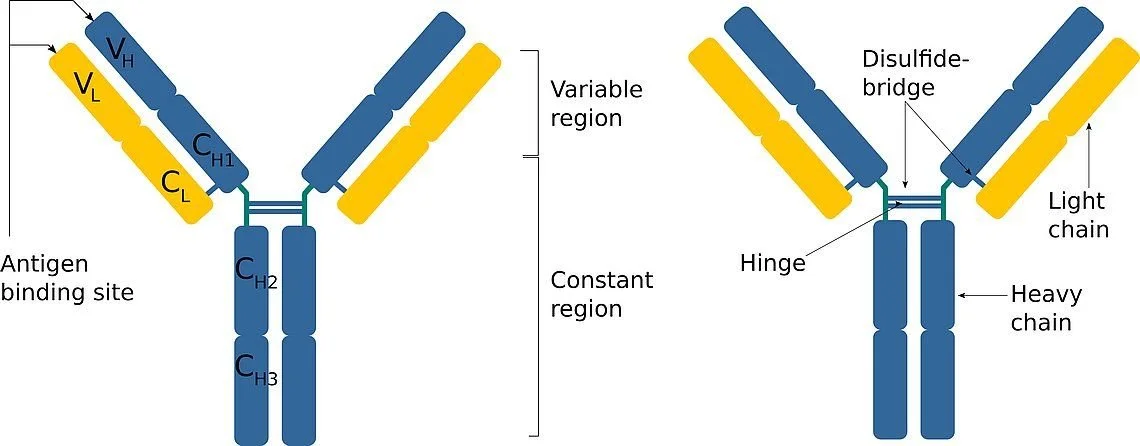
Remember that an antibody has heavy chains (defined by IgG, IgA, and IgM) and light chains (defined by kappa or lambda)
The light chains are the extra elements hanging off the Y shaped antibody
When a B cell develops, it chooses either kappa or lambda for its light chain and your body has a good mix of kappa plasma cells and lambda plasma cells
We can quantify the heavy immunoglobulins in the serum and/or the light chains in the serum
What is a plasma cell dyscrasia?
Abnormal production of a plasma cells that have undergone a mutation that preferentially choose to secrete a specific type of heavy and/or light chains in abundance (monoclonal protein)
Why are excess monoclonal immunoglobulin production bad?
Disruption of osteoclast/osteoblast homeostasis causing lytic lesions
Disruption of erythropoiesis in the bone marrow resulting in anemia
Excess immunoglobulin deposition or light chain cast neuphropathy resulting in renal failure
Development of immune mediated neuropathy (Waldenstrom’s Macroglobulinemia)
What is an “SPEP”?
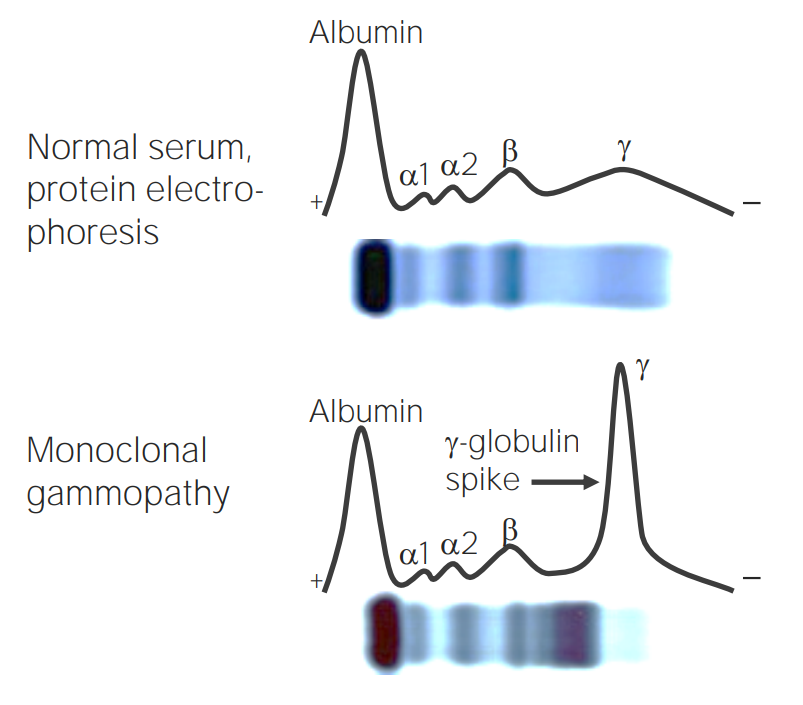
Serum protein electropheresis
The test separates proteins based on size and charge
Normal peaks:
Albumin peak - usually largest peak
Alpha1
Alpha2
Beta - These alpha, beta beaks encompass proteins like the acute phase reactants
Gamma - Gamma is where most of your immunoglobulins will be found. Normally, you want a nice even curve since IGs should be heterogeneous
In a patient with clonal plasma cells, they will start making one particular type of Immunoglobulin over another, therefore you will see a spike in the gamma region
This SPEP curve is interpreted by a pathologist to identify if a “monoclonal spike” or “M-spike” exists in the gamma region
The M-spike can then be quantified (i.e., this is a QUANTITATIVE test; it does not tell us what that protein is)
What is “immunofixation”?
This test is often run in concert with the SPEP (but always check with your lab!), but this is a QUALITATIVE test
Immunofixation helps to identify what the monoclonal protein seen on the SPEP is
What are “serum free light chains”?
TFOC Pro-Tip: If you are ordering an SPEP/IFE, always order serum free light chains!
Important note: Kappa light chains are preferentially cleared by the renal system, therefore in patients with renal dysfunction, you can have abnormal values with a normal kappa/lambda ratio up to 3.1 (see episode 2 in this series)
The light chain values and the ratio have important prognostic information for our patients
For patients with a monoclonal gammopathy, also check urine protein electropheresis (UPEP)!
ALWAYS do 24 hour urine collection (spot is not useful)
This will help us determine if a mild elevation in Cr is more likely related to immunoglobulin deposition if a patient has a large detectable urine M protein for example
This also gives us an idea of the extent of kidney damage as we should not be seeing larger heavy chains in the urine for a normal functioning kidney
Once you have your data, how do you decide if someone has multiple myeloma?
We will discuss this a lot more in our future episodes, but mutliple myeloma is diagnosed when there is a bone marrow biopsy showing >10% clonal plasma cells or biopsy proven plasmacytoma AND myeloma defining events
OR in a patient with a bone marrow biopsy showing >60% plasma cells
Wait, so does everyone with an abnormal SPEP need a bone marrow biopsy?!
NO, see below
What is a monoclonal gammopathy of undetermined significance?
First it is important to know that MGUS is incredibly common in the older adult population and does not mean that a patient has cancer or will develop myeloma
Population based studies have shown a prevalence of MGUS ~3% in adults over the age of 50 and in 6% of the African American population (Kyle et al. NEJM 2006)
Older studied suggested that rate of progression to myeloma is 1% per year for patients with MGUS (Kyle et al. NEJM 2002); we later learned that it is not that simple
Risk of progression to myeloma varies depending on baseline patient characteristics (i.e. how big was the M spike, what was the heavy chain classification, and what was the light chain discordance)
This is why we always need the serum free light chains - so that we can risk stratify the MGUS to see if we need to do a bone marrow biopsy and lytic lesion imaging study
Factors that influence risk of progression to MM (and therefore warrant a bone marrow biopsy):
Type of heavy chain involved (IgG vs. non IgG with non IgG as higher risk)
Quantity of M-spike (>1.5 is higher risk)
Abnormal free light chain ratio
For light chain only MGUS (FLC must be > 8 to be considered higher risk)
If one or more of the criteria above are met, then you do a bone marrow biopsy and either whole body PET/CT or MRI to evaluate for lytic lesions
This is done so that we can identify patients who may already have myeloma or have a very high risk of developing myeloma
Affects surveillance strategies
Calculator: https://qxmd.com/calculate/calculator_148/mgus-prognosis
References:
https://www.nejm.org/doi/full/10.1056/NEJMoa054494: 2006 article from Kyle et al. discussing MGUS prevalence in general population
https://www.nejm.org/doi/full/10.1056/nejmoa01133202: 2002 article from Kyle et al. discussing MGUS progression estimated 1% per year
https://ashpublications.org/blood/article/131/2/163/37011/How-I-manage-monoclonal-gammopathy-of-undetermined: Great review article on MGUS
The crew behind the magic:
Show outline: Vivek Patel
Production and hosts: Ronak Mistry, Vivek Patel, Dan Hausrath
Editing: Vivek Patel
Shownotes, graphics, social media management: Ronak Mistry