Episode 137: Follicular Lymphoma Series, Pt 2. - Front-line Management
This week, we continue our conversation on follicular lymphoma, this time focusing on front line therapy. We discuss how we approach localized and diffuse disease and the data behind why we do what we do.
What is the workup of follicular lymphoma?
Check out the previous episode for a refresher on FNA vs core vs excisional biopsy
Ideally, would obtain excisional biopsy as diagnosis of follicular lymphoma requires assessment of underlying nodal architecture to rule out high risk features
Not all locations are amenable to excisional biopsy! Core biopsy is often sufficient, especially in patients with low symptom burden
Obtain PET/CT for staging and assessment of baseline FDG avidity
Lack of high SUV (< 10) favors more indolent course and makes transformation less likely
This is only a rule of thumb! Relying on SUV is not perfect and excisional biopsy is always preferred over relying on PET scan alone
Some transformed lymphomas will have SUV ~ 9, some classic lymphomas will have SUV > 10
SUV > 20 is highly concerning for large cell transformation
SUV ~ 4–5 is highly likely to be classic follicular lymphoma and core biopsy is sufficient
Baseline labs include CBC with differential, LDH, tumor lysis labs (uric acid and phosphorus), hepatitis B panel, and HIV
Bone marrow biopsy can be prognostic for some patients but is generally not required and most often will not change management, with a couple of exceptions:
1) To confirm stage 1 disease, in which case curative radiation may be an option
2) To help clarify whether cytopenias are secondary to follicular lymphoma or a different etiology
If a patient has multiple sites of nodal involvement, a bone marrow biopsy should not be performed
What is the treatment of localized stage 1 follicular lymphoma?
We no longer use grades 1, 2, 3A, and 3B in follicular lymphoma
Instead the term “classic follicular lymphoma” is used in place of grades 1 to 3A and “follicular large B cell lymphoma” for the entity formerly classified as grade 3B
Grade 3B should be treated with more intensive chemo (i.e. R-CHOP)
Grades 1-3A behave similarly and are treated with less intensive approaches (when treatment is indicated)
For stage 1 follicular lymphoma we have two main options:
Observation
Radiation
There is no evidence for improved overall survival with radiation therapy as opposed to observation
However, radiation could spare patients from needing chemotherapy in the future and provide a durable remission
Radiation would be favored is if the disease is causing local symptoms
Again, when considering radiation therapy, bone marrow biopsy should be considered as if there is bone marrow involvement, radiation may provide durable local control but will not cure the underlying disease
What is the history of early stage follicular lymphoma treatment?
In the 1970s, it became clear that some follicular (“nodular”) lymphoma patients who underwent multiple biopsies at different sites had different histologic features, with a follicular growth pattern in one biopsy specimen and diffuse large cells in another
The patients with diffuse large cells often had rapid progression of previously stable adenopathy with rapid symptom development
This established the concept that follicular lymphoma can transform into aggressive large B cell lymphoma
This is the rationale for biopsying the most FDG avid site on PET/CT and explains why underlying transformed disease can be missed at a site that was not biopsied in a patient with early progression or primary refractory disease
In 1984, Dr. Saul Rosenberg reported on a Stanford cohort of 111 patients from 1961 to 1982
82% of patients were not treated at initial diagnosis
Median overall survival was 11 years (even without modern treatment options!) and some patients lived over 20 years
For patients diagnosed in their 70s and 80s, life expectancy may be shorter than the time to treatment for follicular lymphoma
A follow up study published in JCO 2004 included a Stanford cohort of 43 patients who were all observed initially
Roughly 60% of patients did not need treatment at a median follow up of 7 years
One study published in 1988 compared observation vs. a very aggressive regimen called ProMACE-MOPP (!!) and total nodal irradiation for patients with indolent lymphoma
Over 50% in the observation group did not require treatment and there was no difference in overall survival
There are a few different prognostic scores for follicular lymphoma
The FLIPI score has not panned out as well as the IPI score for diffuse large B cell lymphoma
FLIPI was developed in the pre-rituximab era and does not accurately reflect prognosis for treated in the modern era
FLIPI2 is an updated version that incorporates bone marrow involvement and beta 2 microglobulin but is still not ready to make any treatment decisions
The most frequently cited study regarding treatment of follicular lymphoma is the pivotal GELF study published in JCO 1997 including patients with low tumor burden
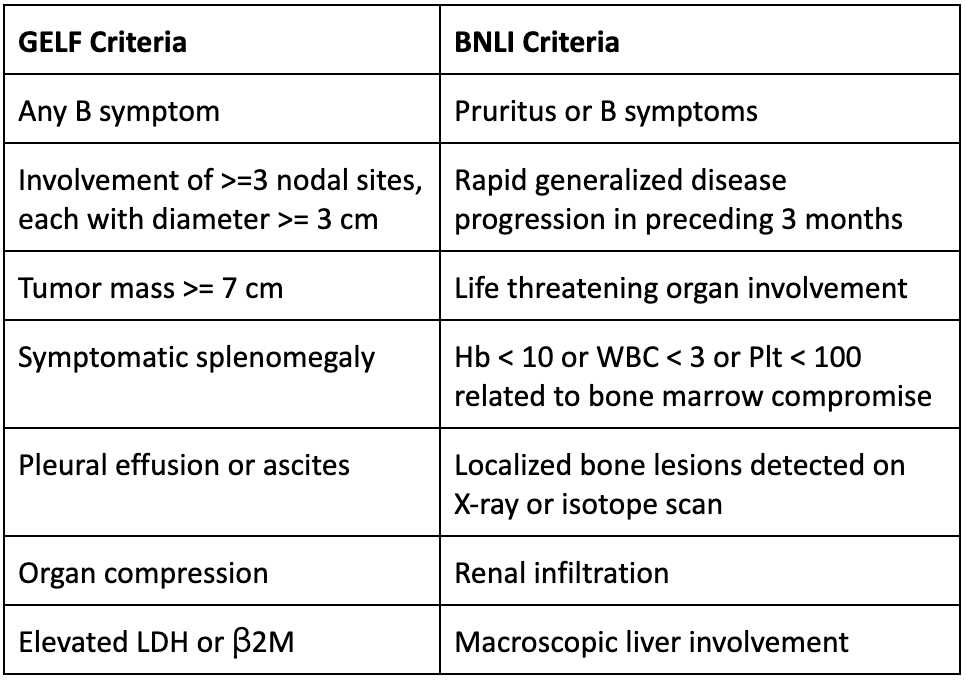
Patients with the features listed in the table below were excluded because they were felt to need treatment
These criteria for treatment in follicular lymphoma have become known as the GELF criteria (GELF is the abbreviation of the French study group)
Patients were randomized 1:1:1 to observation, prednimustine, or interferon
There was no difference in overall survival
Another study published by the BNLI group in Lancet 2003 confirmed these findings in advanced stage follicular lymphoma patients
There were exclusion criteria similar to GELF, listed in the table above
Patients were randomized to watchful waiting vs. chlorambucil
Again, there was no difference in overall survival
Based on the GELF and BNLI studies, observation is the standard of care for patients with follicular lymphoma who do not meet criteria for treatment
Keep in mind that these are only guidelines!
Some patients who meet GELF adenopathy size criteria but remain asymptomatic can still be observed
Conversely, some patients who do not meet criteria may still warrant treatment
What is the data regarding curative intent radiation in localized stage I follicular lymphoma?
Follicular lymphoma is a radiosensitive disease
One pivotal study published in 2006 looked at 106 patients who underwent radiotherapy for early stage, grade 1-2 follicular lymphoma
At 15 year follow up, around 40% of patients remained in remission
It is unclear if the same number of patients would have required treatment, based on the 2004 Stanford study study mentioned earlier
There is a subset of patients who can be cured with radiation and this can prevent the need for systemic therapy in the future
Patients should understand that if they were to continue observation, they might never need treatment
Modern radiation treatments are often 12 fractions x 200 cGy = 24 Gy total
Given the clear local control benefit, radiation is of particular interest if there is involvement of a sensitive area like the spine
What is the treatment of patients with stage III-IV follicular lymphoma who do not meet treatment criteria?
For patients with stage III-IV follicular lymphoma, the GELF and BNLI criteria can be utilized
For patients meriting treatment, options include chemoimmunotherapy (i.e. bendamustine + rituximab or rituximab + lenalidomide) or rituximab monotherapy
There was a randomized study first published in Lancet Oncology in 2014 comparing weekly rituximab (for four doses) followed by maintenance (every two months for two years) vs. weekly rituximab without maintenance vs. observation
The no-maintenance rituximab arm was closed early due to low accrual and the belief that maintenance should be standard of care (likely premature)
There were over 180 patients in the observation arm, 80 in the no-maintenance rituximab arm, and 190 in the rituximab maintenance arm
The proportion of patients not needing treatment at 15 years was 65% in the rituximab maintenance arm, 50% in the no-maintenance rituximab arm, and 35% in the observation arm
There was no difference in time to second treatment nor in overall survival
Of the patients who needed treatment in the observation group, the vast majority received chemotherapy with rituximab (not just rituximab monotherapy)
The authors’ conclusion was that rituximab with maintenance delayed time to treatment and prevented patients from requiring treatment with chemotherapy
Interpretation of this study can be tricky!
Given the lack of improvement in overall survival, there is significant cost and time toxicity associated with coming to infusion clinic every two weeks for two years
Unfortunately, due to closing early, there is an insufficient number of patients in the no-maintenance rituximab arm to draw conclusions about long-term efficacy
Ultimately, in practice, weekly rituximab x 4 doses (without maintenance) is a very reasonable treatment option and it seems that half of patients can avoid further treatment at the 15 year mark (again, keep in mind that 35% would have avoided treatment anyway!)
This is particularly true for patients with symptomatic adenopathy with diffuse disease or are not good candidates for radiation
However, rituximab maintenance is likely not worthwhile for the majority of patients
What are the chemoimmunotherapy options for patients with stage III-IV follicular lymphoma?
There were historically three common chemotherapy regimens in the rituximab era:
Bendamustine + rituximab
R-CHOP (rituximab + cyclophosphamide + doxorubicin (hydroxydaunorubicin) + vincristine (Oncovin) + prednisone)
R-CVP (no anthracycline: rituximab + cyclophosphamide + vincristine + prednisone)
BR has much less toxicity than R-CHOP
Two phase 3 randomized trials demonstrated non inferiority and possible superiority of BR over R-CHOP or R-CVP
The STiL study conducted in Germany was published in 2013 and showed improved progression free survival with BR over R-CHOP but there was no difference in overall survival
The BRIGHT study conducted in the United States was published in 2014 and showed a similar PFS and OS between BR vs. investigator’s choice (R-CHOP or R-CVP)
In both studies, BR was less toxic
As a result of these studies, BR became standard of care
The complete response rate was ~60%, yet the progression free survival was around 50% at 9-10 years
This shows that a complete response is not necessary! Debulking is often good enough in this indolent disease
This is helpful context to keep in mind when evaluating newer bispecific antibody therapy, which can have CR rates up to 90%
The RELEVANCE phase 3 randomized trial published in NEJM 2018 evaluated R2 (lenalidomide (Revlimid) + rituximab) vs. investigator’s choice (R-CHOP or R-CVP) and showed non inferiority of the R2 regimen
What about R2 vs BR?
There has never been a study comparing these two regimens
R2 is an expensive regimen and involves eighteen months of treatment (compared to only six months for BR)
Additionally, R2 is approved in the second line and is effective in this setting
What is the role of bone marrow biopsies in follicular lymphoma?
A pooled analysis published in JCO 2023 including 580 patients with untreated follicular lymphoma to assess whether initial bone marrow biopsy affected outcomes
Only 5/580 (0.9%) had positive baseline bone marrow biopsy, complete response on imaging, and subsequent positive bone marrow biopsy
In other words, for 99% of patients, bone marrow biopsy was irrelevant to response
Therefore, the role of bone marrow biopsy in follicular lymphoma should be limited to patients who are candidates for curative radiation (to rule out systemic involvement) and to patients with unexplained cytopenias (to help clarify whether they are related to lymphoma or a different etiology)
What is the data regarding rituximab maintenance?
The PRIMA trial evaluated over 1000 patients who (after response to chemoimmunotherapy induction) were randomly assigned to two years of rituximab maintenance (every 8 weeks) vs observation
Time to next treatment was 50% in the rituximab maintenance arm vs 40% in the observation arm
There was no difference in overall survival
Rituximab maintenance can be offered, but given the modest PFS benefit, it is likely not worthwhile for the majority given cost and time toxicity
The most important prognostic factor in follicular lymphoma is progression within 24 months (POD24), which occurs in ~20% of patients
Newer, better therapies such as bispecific antibodies are now available
The next treatment might be radiation or rituximab monotherapy for patients with low burden disease
What are the take-home points?
Localized stage I follicular lymphoma: Observation vs. curative intent radiation
Advanced stage III-IV follicular lymphoma not meeting criteria for treatment: Observation vs. rituximab monotherapy
Advanced stage III-IV follicular lymphoma meeting criteria for treatment: BR vs. R-CHOP (or R-CVP)
The crew behind the magic:
Show outline: Vivek Patel
Production and hosts: Ronak Mistry, Vivek Patel, Dan Hausrath
Editing: Resonate Recordings
Shownotes: Neil Biswas
Social media management: Ronak Mistry
We are proud to partner with HemOnc.org!
Want to learn more about the trials that lead to the regimens discussed today? What about dosing schedules? See links in the show notes for a link to HemOnc.org
Have some extra time and want to make some extra money? Click here to get paid to participate in market research surveys!