Episode 134: VTE Series - Diagnosis of Antiphospholipid Antibody Syndrome
This week, we continue our series focusing on venous thromboembolism. In this episode, we begin our discussion of antiphospholipid syndrome.
What is antiphospholipid syndrome (APS)?
Check out Episode 132 for a reminder of when to order hypercoagulability testing
Antiphospholipid antibodies are not synonymous with antiphospholipid (antibody) syndrome and lupus anticoagulant is not synonymous with lupus (SLE)!
APS is a systemic autoimmune disease that is characterized by thrombotic or obstetric complications in the presence of persistently positive antiphospholipid antibodies
Often associated with other autoimmune diseases, but not always
There are three main antibodies implicated in APS:
Lupus anticoagulant
Anticardiolipin antibodies
Anti-beta-2 glycoprotein antibodies
These antibodies target beta-2-glycoprotein I, a plasma protein that binds to phospholipids. This promotes dimerization, which then causes an upregulation of prothrombotic cell adhesion molecules, decreased tissue factor pathway inhibitor, decreased protein C activity, and activation of complement
The presence of these antibodies increases the risk for both venous and arterial thromboembolic events, which is unique!
What is the prevalence of antiphospholipid antibodies?
There are no good population-based studies to evaluate this
One study evaluating healthy blood donors found that 10% of people had positive anticardiolipin antibodies and 1% were positive for lupus anticoagulant
In most patients, less than 1% will still be positive in one year
The prevalence in other groups is likely higher. One analysis suggested antibodies were present in:
20-30% of lupus patients
6% of patients with pregnancy complications with no history of autoimmune disease
10% of patients with thrombosis
11% of patients with myocardial infarction
17% of patients with strokes under the age of 50
It is important to note that these studies included patients who were positive once, but antibodies were never rechecked and/or patients were borderline positive
Borderline positive antibody levels (in isolation) are not clinically meaningful!
More common in women than men
Which patients should be screened for APS?
Younger patients (< 50 years of age) who have unexplained thrombotic events (venous or arterial) or microvascular disease (end organ dysfunction or evidence of vascular compromise)
Patients who have adverse outcomes related to pregnancy (severe preeclampsia or placental insufficiency)
Livedo reticularis
Valvular heart disease (specifically non-bacterial thrombotic endocarditis)
Pulmonary hemorrhage
Thrombotic microangiopathy affecting the kidney
Neurologic findings with cognitive deficits and white matter lesions
Any of the above findings in background of systemic lupus erythematosus
There can also be abnormal labs that can raise suspicion:
Prolonged aPTT
False positive VDRL or RPR
Unexplained thrombocytopenia (however, most clinicians do not order this for thrombocytopenia alone)
When should APS workup be ordered?
Practice patterns vary by institution
There is a possibility of false positive testing in the setting of acute thrombosis
Some clinicians prefer to test in the inpatient setting as it can influence the choice of anticoagulation on discharge
Remember that testing has to be repeated in 12 weeks to confirm results!
Normal aPTT does not rule out APS!
What is the history of APS?
In the 1960s, hematologists observed the "lupus anticoagulant," an antibody associated with blood clotting
APS was not recognized until the 1980s, when researchers identified anticardiolipin antibodies (aCL) and their link to thrombosis and pregnancy loss
Observational Period (1960s–1983): Reports described clotting abnormalities in patients with lupus
Exponential Growth (1983–1995): Anticardiolipin test was developed, leading to a surge in APS research. However, the methodology to perform this assay was not uniform, leading to a push to standardize the assay
In the 1980s, a committee within the International Society on Thrombosis and Hemostasis (ISTH) was formed. Eventually it was identified that IgM and IgG were the isotypes that were associated with thrombotic events.
There was also a new discovery in the early 1990s that showed that beta-2 glycoprotein I plays an important role in this process.
Refinement and Classification (1995–Present): In 1999, experts gathered in Sapporo in an effort to standardize the definition of this syndrome. They required one of two clinical criteria (either pregnancy loss or thrombosis) and one of two lab criteria (positive IgG or IgM anticardiolipin at levels > 40 and/or positive lupus anticoagulant) which had to be positive at least twice at least 8 weeks apart
In 2006, the criteria was updated (aka Sydney Criteria or Revised Sapporo Criteria). They added IgG and IgM beta-2 glycoprotein I and adjusted the time frame to at least 12 weeks apart
In 2023, the American College of Rheumatology and the European Alliance of Associations for Rheumatology created a new definition with a significantly more extensive list of criteria. This was an attempt to include more patients in rheumatologic studies related to APS. However, these have not been regularly used by hematologists.
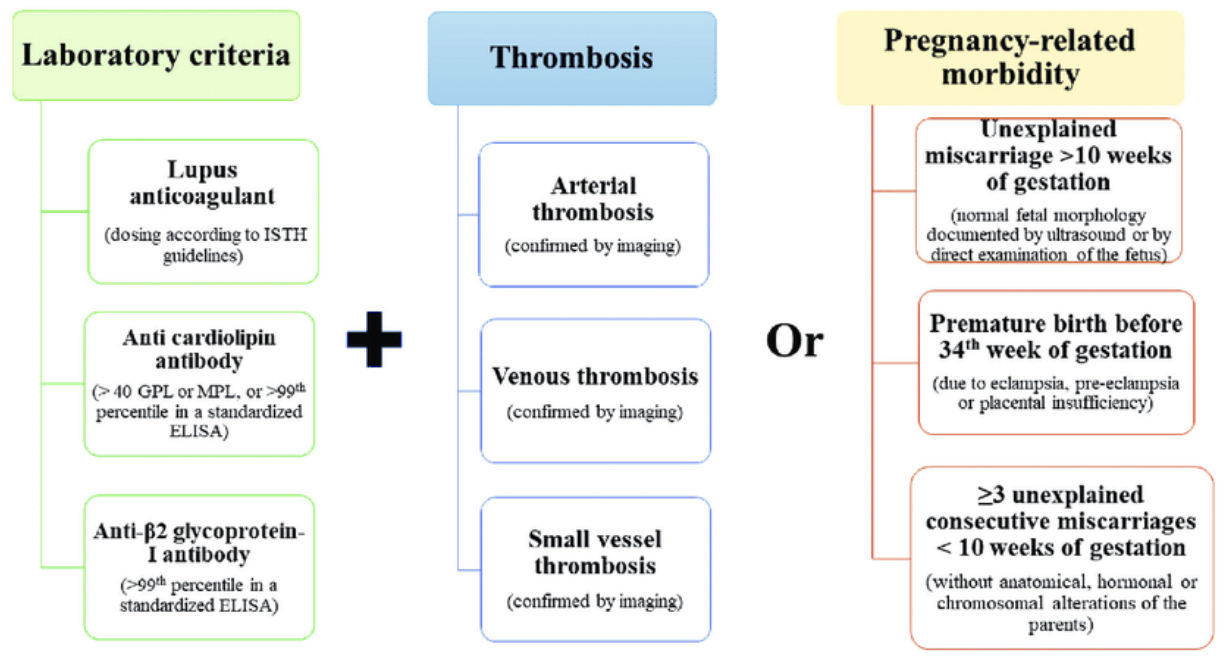
What is the current definition of antiphospholipid antibody?
There are two clinical criteria:
Vascular thrombosis: One or more arterial, venous, or small vessel thrombosis (not superficial venous thrombosis)
Pregnancy morbidity: One or more unexplained deaths of a morphologically normal fetus at or beyond the 10th week of gestation with normal fetal morphology documented by ultrasound or by direct examination
Pregnancy morbidity can also include one or more premature births of a morphologically normal neonate before the 34th week of gestation due to eclampsia / severe pre-eclampsia or features of placental insufficiency
Pregnancy morbidity can also include three or more unexplained consecutive spontaneous abortions before the 10th week of gestation without maternal anatomic or hormonal abnormalities
There are also three laboratory criteria:
Lupus anticoagulant present in plasma on two occasions at least 12 weeks apart
Anticardiolipin antibody IgG and/or IgM in serum or plasma in high antibody titers (>40 GPL/MPL or > 99th percentile) on two or more occasions at least 12 weeks apart
Anti-beta-2 glycoprotein I antibody IgG and/or IgM in high antibody titers on two or more occasions at least 12 weeks apart
There is also ACR/EULAR criteria, although they are not as widespread: https://ard.bmj.com/content/82/10/1258
Image source: Pignatelli et al. “Seronegative antiphospholipid syndrome.” Haematologica vol. 105,3 (2020): 562-572. No copyright infringement intended.
How are these tests performed?
The anticardiolipin and beta-2-glycoprotein IgM/IgG assays are ELISA tests and anticoagulation should not affect the results
However, lupus anticoagulant is a functional assay like the aPTT test; as such, the presence of anticoagulants can make tests false positive or false negative
It is preferable to test for APS off anticoagulation (especially DOACs) but oftentimes this is not feasible. Warfarin does not completely stop the function of proteins but rather decreases clotting protein production; therefore, a mixing study would fix the deficiency induced by warfarin
Additionally, lupus anticoagulant can also be positive due to acute phase reactants
Specifically, a positive lupus anticoagulant requires demonstration of a prolonged phospholipid-dependent screening test such as a dilute Russell viper venom time (dRVVT) or PTT-LA
These assays use low phospholipid environments and are thus more sensitive to a lupus anticoagulant - if there is any lupus anticoagulant present, it will cause a prolonged test because there will not be an excess phospholipids
Mixing patient plasma fails to correct the prolonged screening tests, which suggests an inhibitor rather than a coagulation factor deficiency
Addition of excess phospholipids corrects the test, suggesting phospholipid dependence
The test can usually be done on warfarin because a mixing study can be done to replace the clotting factors. However, it cannot be done on a DOAC because there is an inhibitor of factor Xa that cannot be overcome
https://www.islh.org/web/downloads/2020-LAC-guidance-JTH-16859413.pdf
Image source: Tripodi A. Diagnostic Challenges on the Laboratory Detection of Lupus Anticoagulant. Biomedicines. 2021;9(7):844. Published 2021 Jul 20. No copyright infringement intended.
What are some key points to remember?
Both clinical and laboratory findings are required to have a diagnosis of APS
The antibody titers do matter so always ask if they are not provided (IgA does not matter)
Until the patient has repeat testing and it is proven that antibodies are present at least 12 weeks apart, the patient does not have an official diagnosis of antiphospholipid antibody syndrome
The crew behind the magic:
Show outline: Ronak Mistry
Production and hosts: Ronak Mistry, Vivek Patel, Dan Hausrath
Editing: Resonate Recordings
Shownotes: Neil Biswas
Social media management: Ronak Mistry
We are proud to partner with HemOnc.org!
Want to learn more about the trials that lead to the regimens discussed today? What about dosing schedules? See links in the show notes for a link to HemOnc.org
Have some extra time and want to make some extra money? Click here to get paid to participate in market research surveys!